Condition Basics
What is bronchitis?
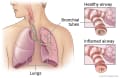
Bronchitis means that the tubes that carry air to the lungs (the bronchial tubes) are inflamed and irritated. When this happens, the bronchial tubes swell and produce mucus. This makes you cough.
There are two types of bronchitis:
- Acute Bronchitis usually comes on quickly and gets better after 2 to 3 weeks. Most healthy people who get acute bronchitis get better without any problems. But it can be more serious in older adults and children and in people who have other health problems such as asthma or COPD. Complications can include pneumonia and repeated episodes of severe bronchitis.
- Chronic bronchitis keeps coming back and can last a long time, especially in people who smoke. Chronic bronchitis means that you have a cough with mucus most days of the month for 3 months of the year and for at least 2 years in a row.
What causes acute bronchitis?
Acute bronchitis is usually caused by a virus. Often a person gets it a few days after having an upper respiratory tract infection such as a cold or the flu. Sometimes it is caused by bacteria. It also can be caused by breathing in things that irritate the bronchial tubes, such as smoke.
What are the symptoms?
The main symptom of acute bronchitis is a cough that usually is dry and hacking. After a few days, the cough may bring up mucus. You may have a low fever and feel tired. Most people get better in 2 to 3 weeks. But some people have a cough for more than 4 weeks.
How is it diagnosed?
Your doctor will ask you about your symptoms and examine you. This usually gives the doctor enough information to find out if you have acute bronchitis.
In some cases, you may need a chest X-ray or other tests. These tests are to make sure that you don't have pneumonia, whooping cough, or another lung problem. This is especially true if you've had bronchitis for a few weeks and aren't getting better. More testing also may be needed for babies, older adults, and people who have lung disease (such as asthma or COPD) or other health problems.
How is acute bronchitis treated?
Most people can treat symptoms of acute bronchitis at home. They don't need antibiotics or other prescription medicines. Antibiotics don't help with viral bronchitis. And even bronchitis caused by bacteria will usually go away on its own.
If you have signs of bronchitis and have heart or lung disease (such as heart failure, asthma, or COPD) or another serious health problem, talk to your doctor right away. You may need treatment with antibiotics or medicines to help with your breathing. Early treatment may prevent problems, such as pneumonia or repeated cases of acute bronchitis caused by bacteria.
How can you care for yourself at home?
When you have acute bronchitis, there are things you can do to feel better.
- Don't smoke.
If you need help quitting, talk to your doctor about stop-smoking programs and medicines. These can increase your chances of quitting for good.
- Suck on cough drops or hard candies to soothe a dry or sore throat.
Cough drops won't stop your cough, but they may make your throat feel better.
- Breathe moist air from a humidifier, a hot shower, or a sink filled with hot water. Follow the directions for cleaning the humidifier.
The heat and moisture can help keep mucus in your airways moist so you can cough it out easily.
- Ask your doctor if you can take nonprescription medicine.
This may include acetaminophen, ibuprofen, or aspirin to relieve fever and body aches.
Don't give aspirin to anyone younger than age 20. It has been linked to Reye syndrome, a serious illness. Be safe with medicines. Read and follow all instructions on the label.
- Rest more than usual.
- Drink plenty of fluids so you don't get dehydrated.
- Use an over-the-counter cough medicine if your doctor recommends it.
Cough suppressants may help you to stop coughing. Expectorants can help you bring up mucus when you cough.
Cough medicines may not be safe for young children or for people who have certain health problems.