Breast Cancer Screening
Tests are used to screen for different types of cancer when a person does not have symptoms.
Scientists study screening tests to find those with the fewest harms and most benefits. Cancer screening trials also are meant to show whether early detection (finding cancer before it causes symptoms) helps a person live longer or decreases a person's chance of dying from the disease. For some types of cancer, the chance of recovery is better if the disease is found and treated at an early stage.
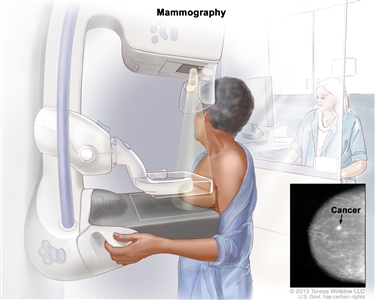
Mammography is the most common screening test for breast cancer.
A mammogram is a picture of the inside of the breast. Mammography may find tumors that are too small to feel. It may also find ductal carcinoma in situ (DCIS). In DCIS, abnormal cells line the breast duct, and in some women may become invasive breast cancer.
There are different types of mammograms:
- Screen-film mammography (SFM) is an x-ray picture of the breast.
- Digital mammography (DM) is a computer picture of the breast.
- Digital breast tomosynthesis (DBT) uses x-rays to take a series of pictures of the inside of the breast from many different angles. A computer is used to make 3-D pictures of the breast from these x-rays.
- Synthetic 2-dimensional mammography (S2D) uses x-rays to take pictures of the inside of the breast, usually from two different angles. A computer or x-ray film is used to make 2-D pictures of the breast.
Digital breast tomosynthesis (DBT) was approved by the U.S. Food and Drug Administration (FDA) in 2018 and is now used in 3 out of 4 facilities. One recent study found that synthetic 2-dimensional mammography (S2D) combined with DBT improved tumor detection rates and lowered mammogram callbacks, radiation dose, and overall costs. More studies are being done to compare different types of breast cancer screening.
Mammography is less likely to find breast tumors in women with dense breast tissue. Because both tumors and dense breast tissue appear white on a mammogram, it can be harder to find a tumor when there is dense breast tissue. Younger women are more likely to have dense breast tissue. To learn more, visit Dense Breasts: Answers to Commonly Asked Questions.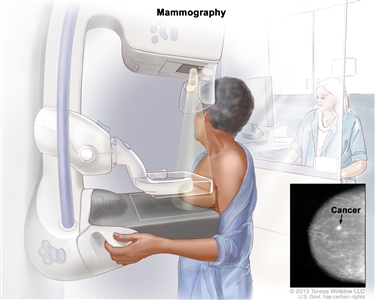
Mammography. The breast is pressed between two plates. X-rays are used to take pictures of breast tissue.
Many factors affect whether mammography is able to detect (find) breast cancer:
- The age and weight of the patient.
- The size and type of tumor.
- Where the tumor has formed in the breast.
- How sensitive the breast tissue is to hormones.
- How dense the breast tissue is.
- The timing of the mammography within the woman's menstrual cycle.
- The quality of the mammogram picture.
- The skill of the radiologist in reading the mammogram.
Women aged 50 to 69 years who have screening mammograms have a lower chance of dying from breast cancer than women who do not have screening mammograms.
Fewer women are dying of breast cancer in the United States, but it is not known whether the lower risk of dying is because the cancer was found early by screening or whether the treatments were better.
Magnetic resonance imaging (MRI) may be used to screen women who have a high risk of breast cancer.
MRI is a procedure that uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the body. This procedure is also called nuclear magnetic resonance imaging (NMRI). MRI does not use any x-rays, and the woman is not exposed to radiation. 
An MRI of the breast is a procedure that uses radio waves, a strong magnet, and a computer to create detailed pictures of the inside of the breast. A contrast dye may be injected into a vein (not shown) to make the breast tissues easier to see on the MRI pictures. An MRI may be used with other breast imaging tests to detect breast cancer or other abnormal changes in the breast. It may also be used to screen for breast cancer in some people who have a high risk of the disease. Note: The inset shows an MRI image of the insides of both breasts. Credit for inset: The Cancer Imaging Archive (TCIA).
MRI may be used as a screening test for women who have a high risk of breast cancer. Factors that put women at high risk include:
- Certain gene changes, such as changes in the BRCA1 or BRCA2 gene.
- A family history of breast cancer in a first-degree relative, such as a mother, daughter, or sister.
- Certain genetic syndromes, such as Li-Fraumeni syndrome or Cowden syndrome.
An MRI is more likely than mammography to find a breast mass (lump) that is not cancer.
Women with dense breasts who have supplemental screening (for example, an MRI) show higher rates of breast cancer detection, but there is limited evidence about whether this leads to better health outcomes.
Whether a woman should be screened for breast cancer and the screening test to use depends on certain factors.
Women with risk factors for breast cancer, such as certain changes in the BRCA1 or BRCA2 gene or certain genetic syndromes, may be screened at a younger age and more often.
Women who have had radiation treatment to the chest, especially at a young age, may start routine breast cancer screening at an earlier age. The benefits and risks of mammograms and MRIs for these women have not been studied.
Breast cancer screening has not been shown to benefit the following women:
- Older women who, if diagnosed with breast cancer through screening, will usually die of other causes. Screening mammograms for those aged 66 to 79 years may find cancer in a very small percentage of women, but most of these cancers are low risk.
- In women with an average risk of developing breast cancer, screening mammography before age 40 has not shown any benefit.
- In women who are not expected to live for a long time and have other diseases or conditions, finding and treating early-stage breast cancer may reduce their quality of life without helping them live longer.
Other screening tests have been or are being studied in clinical trials.
Studies have been done to find out if the following breast cancer screening tests are useful in finding breast cancer or helping women with breast cancer live longer.
Breast exam
A clinical breast exam is an exam of the breast by a doctor or other health professional. He or she will carefully feel the breasts and under the arms for lumps or anything else that seems unusual. It is not known if having clinical breast exams decreases the chance of dying from breast cancer.
Breast self-exams may be done by women or men to check their breasts for lumps or other changes. If you feel any lumps or notice any other changes in your breasts, talk to your doctor. Doing regular breast self-exams has not been shown to decrease the chance of dying from breast cancer.
Thermography
Thermography is a procedure in which a special camera that senses heat is used to record the temperature of the skin that covers the breasts. Tumors can cause temperature changes that may show up on the thermogram.
There have been no randomized clinical trials of thermography to find out how well it detects breast cancer or the harms of the procedure.
Tissue sampling
Breast tissue sampling is taking cells from breast tissue to check under a microscope. Breast tissue sampling as a screening test has not been shown to decrease the risk of dying from breast cancer.
Ultrasound exam
A procedure in which high-energy sound waves are bounced off internal tissues or organs and make echoes. The echoes form a picture of body tissues called a sonogram.
An ultrasound is sometimes used as an additional screening test for women who are at increased risk of developing breast cancer (such as women with dense breasts). It is not known if supplemental screening with ultrasound leads to better health outcomes.
Screening tests for breast cancer are being studied in clinical trials.
Information about clinical trials supported by NCI can be found on NCI's clinical trials search webpage. Clinical trials supported by other organizations can be found on the ClinicalTrials.gov website.