Shop for Plans
Shop for your own coverage
Plans through your employer
Learn about the medical, dental, pharmacy, behavioral, and voluntary benefits your employer may offer.
Learn
Living or working abroad?
Nutrition in Cancer Care: Supportive care - Patient Information [NCI]
What is nutrition?
Nutrition is what you eat and drink and how your body uses it. Good nutrition is important for good health. A healthy diet includes a variety of foods and liquids that have nutrients (vitamins, minerals, proteins, carbohydrates, fats, and water) your body needs.
Good nutrition for people with cancer may differ from what we think of as healthy
People with cancer often need to follow diets that are different from what we think of as healthy. For most people, a healthy diet includes lots of whole grains, fruits and vegetables, modest amounts of protein, and small amounts of sugar, alcohol, salt, and unhealthy fats.
When you have cancer, though, you may need extra protein and calories. To eat enough protein and calories, your diet may need to include more meat, fish, eggs, dairy, fats, and plant-based proteins than someone without cancer. The extra protein and calories will help you keep your strength up to deal with the side effects of treatment, prevent malnutrition, and maintain your best possible quality of life.
A registered dietitian can help make sure you get the right amount of protein and calories during and after cancer treatment. They will work with you, your family, and the rest of your medical team to help manage your diet.
Plan nutrition before cancer treatment
During treatment, you may be tired and not feel well. Being tired can make it harder to grocery shop, cook, and eat. Planning meals before treatment will make it easier to eat during treatment.
To plan meals and snacks before treatment, try these tips.
Shopping tips:
- Fill the refrigerator, pantry, and freezer with healthy foods, especially those high in protein and calories.
- Stock up on foods that need little or no cooking, such as frozen foods.
- Use online grocery shopping and save your list for easy reordering.
- Use delivery or shop-from-home grocery stores.
Meal prep tips:
- Keep
easy-to-digest snacks on hand for when you feel sick. Pretzels and crackers are good examples. - Cook foods ahead of time and freeze them in meal-sized portions.
Tips for accepting help from others:
- Ask friends or family to help you shop and cook during treatment.
- If people offer to grocery shop for you, let them.
- Create a grocery list of items to give to friends and family.
Effects of cancer treatment on nutrition
Both cancer and cancer treatments may cause side effects that affect your taste, smell, appetite, and ability to eat enough food or absorb the nutrients from food. This can lead to malnutrition.
People with certain cancers are more likely to have problems eating. These cancers include those that affect your digestive system directly, such as cancers of the head and neck, esophagus, stomach, pancreas, liver, or colon. But people with any type of cancer can find it hard to eat well because of the effects of cancer treatment.
When malnutrition is not managed in people having cancer treatment, it can lead to cancer cachexia. Cancer cachexia is a wasting syndrome that can cause weakness, weight loss, and fat and muscle loss. It can occur even when you are eating well.
Learn more about
Chemotherapy and eating problems
Chemotherapy uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing. But these drugs may also kill healthy cells that grow and divide quickly, such as cells in the mouth and digestive tract. This can cause eating problems and other side effects, including:
-
loss of appetite -
nausea and vomiting -
constipation -
diarrhea -
dry mouth -
sores in the mouth or throat -
changes in the way food tastes -
trouble swallowing - feeling full after eating a small amount of food (early satiety)
If you are on chemotherapy, you may have a high risk of infection, including from food (foodborne illness). That is because chemotherapy can reduce the number of your white blood cells, which fight infection. It is important that you and your caregivers
Learn more about
Hormone therapy and eating problems
Hormone therapy may be used to slow or stop cancers that rely on hormones to grow, like breast, ovarian, and prostate cancer. Hormone therapy adds, blocks, or removes these hormones. These drugs can cause weight gain and other side effects, including:
-
fluid retention (edema) - nausea and vomiting
- high blood sugar, also called hyperglycemia
-
fatigue
Learn more about
Immunotherapy and eating problems
Immunotherapy uses your immune system to fight cancer. The side effects of immunotherapy are different for each person and depend on the type of immunotherapy drug.
Immunotherapy may cause fatigue, which can lead to a poor appetite. Learn more about
Common nutrition-related side effects caused by immunotherapy include:
- fever
- nausea and vomiting
- diarrhea
Learn more about
Radiation therapy and eating problems
Radiation therapy kills cancer cells and healthy cells in the area that is being treated.
Radiation therapy to any part of your digestive system has side effects that cause eating problems. Most of the side effects begin 2 to 3 weeks after radiation therapy begins and go away a few weeks after it is finished. But some side effects can last for months or years after treatment ends. Learn more about
Fatigue, which can lead to a poor appetite, is a common side effect of radiation therapy. Learn more about
Radiation therapy to the brain or head and neck may cause:
- loss of appetite
- nausea and vomiting
- dry mouth or thick saliva
- sore mouth and gums
- changes in the way food tastes
- trouble swallowing
- pain when swallowing
- being unable to fully open the mouth
Radiation therapy to the chest may cause:
- loss of appetite
- nausea and vomiting
- trouble swallowing
- pain when swallowing
- choking or breathing problems caused by changes in the upper esophagus
Radiation therapy to the abdomen, pelvis, or rectum may cause:
- nausea and vomiting
- bowel blockage
- inflamed colon
- diarrhea
- radiation enteritis
Learn more about
Stem cell transplant and eating problems
People who have a stem cell transplant have special nutrition needs. Medications used before or during a stem cell transplant may cause side effects that keep you from eating and digesting food as usual.
Common nutrition-related side effects caused by stem cell transplant include:
- mouth and throat sores
- diarrhea
If you have a stem cell transplant, you have a high risk of infection, including from food (foodborne illness). That is because treatment given before your transplant reduces the number of your white blood cells, which fight infection. It is important that you and your caregivers learn about how to safely prepare food and how to avoid foods that may cause infection.
After a stem cell transplant, you are also at risk of acute or chronic graft-versus-host disease (GVHD). GVHD may affect your digestive tract, skin, or liver and change your ability to eat or absorb nutrients from food.
Learn more about
Surgery and eating problems
Surgery is a common part of cancer treatment. Surgery that removes all or part of certain organs can affect your ability to eat and digest food. After any surgery, your body needs extra energy and nutrients to heal wounds, fight infection, and recover. If you are malnourished before surgery, you may have trouble healing.
Common nutrition-related side effects caused by surgery include:
- loss of appetite
- trouble chewing
- trouble swallowing
- feeling full after eating a small amount of food, also known as early satiety
Learn more about
Targeted therapy and eating problems
Targeted therapy is a type of cancer treatment that targets proteins that control how cancer cells grow, divide, and spread. It may disturb normal function of your digestive system and cause:
- constipation
- diarrhea
- nausea and vomiting
- abdominal pain
Other problems might include taste changes and a dry or sore mouth. Learn more about
Food safety during cancer treatment
Some cancer treatments can weaken your immune system. This makes it harder for you to fight infections, including foodborne illnesses. So, you need to take special care in the way you handle and prepare food during your cancer treatment. Keep foods at safe temperatures, scrub raw vegetables and fruits, and be careful to use separate utensils, plates, and cutting boards when preparing meats and produce.
Learn more about risk of
Nutrition screening and assessment during cancer treatment
If you have trouble eating and maintaining your weight, your nurse, doctor, or registered dietitian may ask you a series of questions to find out if you are malnourished or are likely to become so.
To assess your nutrition status, you may be asked about:
- weight changes
- changes in the amount of food you eat
- changes in types of food you eat
- problems with eating, like nausea or vomiting
- your ability to walk or do other daily activities
If you are at risk of poor nutrition or malnutrition, your doctor will refer you to a registered dietitian. A registered dietitian can do an assessment, which reviews your:
- food and diet history
- medication history
- personal, medical, family, and social history
- height and weight
- lab tests
- side effects of treatment
- physical exam
Based on this information, the registered dietitian will create a nutrition care plan. This plan includes ways you and your family can improve your eating and address any nutrition problems that you are having.
Ways to manage nutrition problems caused by cancer treatments
When side effects of cancer or cancer treatment affect normal eating, there are ways to help you get the nutrients you need.
Ways to manage appetite loss, weight loss, and early satiety
If you have loss of appetite, weight loss, or feel full too quickly, these tips may help:
- Eat
foods that are high in protein andcalories . - Eat high-protein foods first in your meal.
- Add extra protein and calories to food.
- Drink most of your fluids between meals, not during meals. Small sips at mealtime are okay.
- Drink milkshakes, smoothies, juices, or soups if you do not feel like eating solid foods.
- Eat foods that smell good.
- Try new foods and new recipes.
- Use a blender to make high-calorie, high-protein drinks.
- Try nutrition supplements, such as Ensure or Boost.
- Aim to eat smaller meals and snacks five to six times a day.
- Eat your largest meal when your appetite is strongest, whether that's breakfast, lunch, or dinner.
- Make and store small amounts of your favorite foods so they are ready to eat when you are hungry.
- Find a physical activity you enjoy and will stick with to help increase your appetite.
If you continue to struggle to eat and keep up your weight, you and your treatment team can discuss other nutrition support options. These options may include
You may also take medicines that increase appetite. Learn more about
Ways to manage nausea and vomiting
Nausea is when you feel sick to your stomach, as if you have the urge to throw up. Vomiting is when you throw up. Nausea and vomiting are common side effects of cancer treatments, including chemotherapy and radiation therapy. But there are medicines that often prevent or relieve nausea and vomiting before they start or become a problem.
When you vomit, you may become dehydrated and lose a lot of electrolytes. Electrolytes are minerals, such as potassium, sodium, and calcium that help balance body fluids and support your heart, nerve, and muscle functions. Talk to your dietitian about which drinks can help prevent dehydration and how much you should drink.
Learn more about
Ways to manage dry mouth
Dry mouth occurs when you have less saliva than you used to. Having less saliva can make it harder to talk, chew, and swallow food. Dry mouth can also change the way food tastes.
Chemotherapy and radiation therapy to the head or neck can damage the glands that make saliva. Immunotherapy and some medicines can also cause dry mouth.
If you have dry mouth:
- Moisten food with sauce, salsa, gravy, or salad dressing.
- Eat
foods that are easy to swallow . - Try eating foods and drinks that are very sweet or tart, such as lemonade, to help make more saliva.
- Chew sugar-free gum or suck on sugar-free hard candy, ice pops, or ice chips.
- Sip water throughout the day.
- Drink 8 or more cups of water each day.
- Swish and spit with carbonated beverages to remove dry or thick saliva.
- Keep your lips moist with lip balm.
- Floss your teeth every day.
- Ask your doctor about special mouthwashes for dry mouth.
- Do not:
- use tobacco products
- inhale secondhand smoke
- use electronic cigarettes
- drink any type of alcohol
- eat foods that hurt your mouth (such as spicy, sour, salty, hard, or crunchy foods)
Talk with your doctor or dentist about using artificial saliva or a similar product to coat, protect, and moisten your mouth and throat.
Ways to manage mouth sores
Cancer treatments can harm fast-growing cells in your mouth. Radiation therapy to the head or neck, chemotherapy, and immunotherapy can cause mouth sores (little cuts or ulcers in your mouth) and tender gums. Dental problems or mouth infections, such as thrush, can also make your mouth sore. Visit a dentist at least 2 weeks before starting immunotherapy, chemotherapy, or radiation therapy to the head and neck.
Your mouth and gums will most likely feel better once cancer treatment ends.
If you have mouth sores:
- Eat soft
foods that are easy to chew . - Cook foods until soft and tender.
- Cut food into small pieces.
- Use a blender or food processor to make food smooth.
- Suck on ice chips to numb and soothe your mouth.
- Eat foods cold or at room temperature. Hot foods can hurt your mouth.
- Drink with a straw to move liquid past the painful parts of your mouth.
- Use a small spoon to help you take smaller bites, which are easier to chew.
- Check your mouth each day for sores, white patches, or puffy and red areas.
- Rinse your mouth three to four times a day. Mix ¼ teaspoon baking soda, ⅛ teaspoon salt, and 1 cup warm water for a mouth rinse.
- Talk to your doctor about medicine to numb your mouth. This may make eating easier.
- Avoid:
- citrus fruits, such as oranges, lemons, and limes
- spicy foods
- tomatoes and ketchup
- salty foods
- raw vegetables
- sharp and crunchy foods
- drinks with alcohol
- mouthwash that contains alcohol
- tobacco products
- electronic cigarettes
- toothpicks or sharp objects
Ways to manage sore throat and trouble swallowing
Chemotherapy and radiation therapy to the head and neck can make the lining of your throat inflamed and sore, a problem called esophagitis. It may feel as if you have a lump in your throat or that your chest or throat is burning. You may also have trouble swallowing. These problems may make it hard to eat and cause weight loss.
Some types of chemotherapy and radiation to the head and neck can harm fast-growing cells, such as those in the lining of your throat. Your risk of sore throat, trouble swallowing, or other throat problems depends on:
- how much radiation you are getting
- if you are getting chemotherapy and radiation therapy at the same time
- whether you use tobacco or drink alcohol during cancer treatment
If you have a sore throat or trouble swallowing:
- Eat soft
foods that are easy to chew and swallow . - Moisten food with gravy, sauces, broth, or yogurt.
- Cook foods until soft and tender.
- Cut food into small pieces.
- Use a blender or food processor to make food smooth.
- Eat five or six small meals every day instead of three large meals.
- Eat
foods and drinks that are high in protein andcalories . - Sit upright and bend your head slightly forward when you eat or drink. Stay upright for at least 30 minutes after eating.
- Do not use tobacco or electronic cigarettes.
- Stay away from the foods and drinks that can burn or scratch your throat, such as:
- hot foods and drinks
- spicy foods
- foods and juices that are high in acid, such as citrus, pineapple, and tomatoes
- sharp or crunchy foods
- drinks with alcohol
- carbonated drinks
Talk to your doctor about tube feedings if you cannot eat enough to stay strong.
Ways to manage taste and smell changes
Cancer treatment, dental problems, or the cancer itself can cause changes in your sense of taste or smell. Food may have less taste or certain foods (like meat) may be bitter or taste like metal. Sometimes, foods that used to smell good to you no longer do.
Although there is no way to prevent these problems, there are things you can do to manage them. And often they get better after treatment ends.
Ways to manage a salty taste:
- Try low-sodium or sodium-free seasoning products, like Mrs. Dash.
- Use herbs, spices, and seasonings in place of salt when cooking.
- Pick naturally sweet foods, like fresh or dried fruit.
- Avoid eating out or getting take-out because restaurants often prepare foods with a lot of salt.
- Boil food, as this reduces salty flavors.
- Add a pinch of sugar or honey to foods.
Ways to manage an overly sweet taste:
- Eat more vegetables.
- Add water and ice to dilute sweet juices. Try mixing half juice and half water.
- Eat sour foods, like grapefruit.
- Add a pinch of salt to food to offset the sweetness.
- Add vinegar or citrus to foods to reduce sweetness.
Ways to manage a loss of taste or "off" taste:
- Choose fresh produce.
- Try foods with fruity, tart, or salty flavors.
- Use marinades on meats to add flavor. Marinate the meat in your refrigerator overnight for more flavor.
- Add vinegars, fresh fruit juices, cheese, salad dressing, and sauces to foods.
- Add fresh or dried herbs, like basil, oregano, thyme, rosemary, mint, or sage.
- Add spices, like onion and garlic powder, paprika, ground turmeric, ground ginger, or curry powder.
- Add condiments, like mayonnaise, relish, ketchup, mustard, or salsa.
- Chew food longer to allow more contact with taste buds.
Ways to manage bitter and metallic tastes:
- Use plastic, silicone, wooden, or bamboo silverware.
- Suck or chew on sugar-free candies, mints, or gum.
- Do not buy prepackaged food in metal containers, such as canned beans. Look for cardboard, glass, or plastic packaging.
- Do not drink from metal containers or use metal silverware.
- Try plant-based protein sources, like tofu, nuts, or beans.
- If red meat tastes metallic, try chicken, turkey, or dairy foods.
- Find nonmeat, high-protein recipes in vegetarian, Chinese, or Indian cookbooks.
- Drink sweet or sour beverages, like cherry, cranberry, pineapple, or grape juice.
- Eat fresh and dried fruits, like mango, peaches, watermelon, dates, or figs.
- Add sweetness to foods with a pinch of sugar, honey, or maple syrup.
Ways to manage smell changes:
- Keep foods covered until ready to eat.
- Drink from cups with lids and drink through a straw.
- Turn a kitchen fan on when cooking, or cook outdoors if smells bother you.
- Avoid strong odors, such as brussels sprouts or fish.
- Make or eat foods that don't need to be cooked, such as:
- protein shakes
- protein bars
- smoothies
- cereal with fruit and milk
- pudding
- Greek yogurt parfaits
- sandwiches
Types of nutrition support if you cannot eat
Sometimes, despite your best efforts, you may not be able to eat enough to stay strong. If this happens, nutrition support through a feeding tube may be a good option. Nutrition support helps if you cannot eat or digest enough food to stay nourished. Staying nourished helps increase the chance of receiving treatment without unplanned breaks.
Your doctor or dietitian will discuss nutrition support with you if they think it will help.
There are two types of nutrition support, enteral and parenteral nutrition.
Enteral nutrition
Enteral nutrition gives you nutrients in liquid form through a tube that is placed into the stomach or small intestine. There are two types of feeding tubes:
- A nasogastric tube is inserted through the nose and down the throat into the stomach or small intestine. This is used when nutrition support is needed for only a few weeks.
- A gastrostomy tube is inserted into the stomach, or a jejunostomy tube is inserted into the small intestine through an opening made on the outside of the abdomen. Feeding tubes of this type are usually used for long-term enteral feeding or for people who cannot use a tube in the nose and throat.
The type of formula used is based on your specific nutritional needs. There are formulas for people with special health conditions, such as diabetes, or with other needs, such as observing religious or cultural norms.
Some people can still eat by mouth when using enteral nutrition. Before doing so, it is important to ask your doctor if it is safe for you.
Parenteral nutrition
Parenteral nutrition is used when you cannot take food by mouth or use a feeding tube. Parenteral feeding does not use the stomach or intestines to digest food. Nutrients are given to you directly into the blood through a catheter inserted into a vein. These nutrients include proteins, fats, vitamins, and minerals.
As with enteral feeding, some people can eat by mouth when using parenteral nutrition. Ask your doctor if it is safe to eat by mouth while receiving parenteral nutrition.
The catheter may be placed into a vein in the chest or in the arm.
A central venous catheter is placed beneath your skin and into a large vein in the upper chest. The catheter is put in place by a surgeon. This type of catheter is used for long-term parenteral feeding.
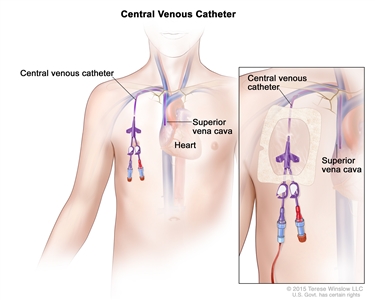
A central venous catheter is a thin, flexible tube that is inserted into a vein, usually below the right collarbone, and guided into a large vein above the right side of the heart called the superior vena cava.
A peripheral venous catheter is placed into your vein in the arm. A peripheral venous catheter is put in place by trained medical staff. This type of catheter is usually used for short-term parenteral feeding or if you do not have a central venous catheter.
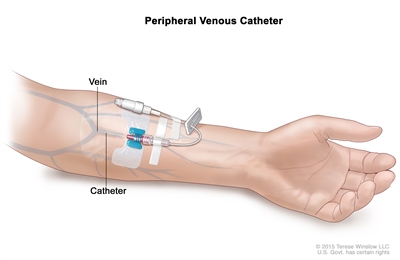
A peripheral venous catheter is a thin, flexible tube that is inserted into a vein. It is usually inserted into the lower part of the arm or the back of the hand.
You will be checked often for infection or bleeding at the place where the catheter enters the body.
Nutrition therapy for the end of life
If you are nearing the end of life, the goal is to provide the best possible quality of life and control symptoms that cause discomfort. Your nutrition goals will be specific to you.
Common symptoms that can occur at the end of life include:
-
loss of appetite -
dry mouth -
swallowing problems -
nausea and vomiting
The focus is on relieving these symptoms, rather than getting enough nutrients.
You and your family can decide how much nutrition and fluids you will be given at the end of life
People at the end of life often do not feel much hunger at all and may want very little food. Sips of water, ice chips, and mouth care can help with thirst. Food and fluids should not be forced on someone who is at the end of life. Doing so can cause discomfort or choking.
You and your loved ones have the right to make informed decisions. Your religious and cultural preferences may affect your decisions. The health care team and a registered dietitian can explain nutrition needs and the benefits and risks of using tube feeding or IV nutrition at the end of life.
Possible benefits of nutrition support for people expected to live longer than a month include:
- improved quality of life
- less risk of death due to malnutrition
- fewer physical and mental problems
The risks of nutrition support at the end of life include:
- bacteria or toxins in the blood or tissues (known as sepsis) with the use of parenteral nutrition
- accidental breathing in of food or fluid into the lungs (known as aspiration) with the use of enteral nutrition
- sores and breakdown of the skin where the enteral feeding tube is inserted
- diarrhea with the use of enteral and parenteral nutrition
- problems caused by too much fluid in the blood with the use of enteral and parenteral nutrition
Appetite loss, weight loss, and cancer
Appetite loss and weight loss are common side effects of cancer and cancer treatments. Anyone with cancer might lose their appetite and lose weight. But you are more likely to lose weight if you have head and neck, lung, pancreatic, or liver cancer or cancer in the upper digestive system. Upper digestive system cancers include cancers in the throat, esophagus, stomach, and the first part of the small intestine.
Appetite loss often leads to eating less than your body needs, which leads to weight loss. Weight loss can also occur when you burn more calories than you are taking in. Weight loss can lead to
Although cachexia also causes weight loss, cachexia and weight loss are different and treated differently. Learn more at
Side effects of cancer treatment that cause problems with eating include:
-
nausea and vomiting -
diarrhea -
constipation - feeling full quickly (early satiety)
-
painful swallowing -
mouth sores -
dry mouth -
taste changes
Other factors that may cause appetite loss and weight loss during cancer treatment include anxiety,
Ways to manage appetite loss and weight loss in people with cancer
If you start to lose your appetite, talk with your doctor or registered dietitian. Speak with them right away if you start to lose weight. Your dietitian can help you and your family manage your weight loss. Here are some tips that may help.
Tips about foods to eat:
- Eat
foods high in protein andcalories . - Add whole milk to hot or cold cereal.
- Eat foods that smell good.
- Try new foods and recipes.
Tips on when to eat:
- Eat small meals every 2 to 3 hours, about 5 or 6 meals per day.
- If you forget it's time to eat, set an alarm to remind yourself.
- Eat within 1 hour of waking up.
- Eat
high-protein foods first in your meal when your appetite is strongest. - Use TV shows, commercial breaks, or radio ads to remember to eat or drink.
- Eat a bedtime snack.
Tips about when and what to drink:
- Drink
liquids between meals to help you stay hydrated. - During meals, sip only small amounts of fluids so you can eat more food.
- Drink milkshakes, smoothies, juices, or soups if you do not feel like eating solid foods.
- Use whole milk or yogurt for milkshakes or smoothies to increase calories.
- Sip on nutrition supplement drinks between meals. Examples include Ensure and Boost.
Meal prep tips:
- Make and store small amounts of your favorite foods so they are ready to eat.
- Add full-fat cheese to toast, eggs, crackers, soups, pasta, and potatoes.
- Add creamy sauces to pasta and other dishes.
- Add leftover meat to eggs, salad, pasta, and soups.
- Add beans and lentils to soup, salad, pasta, tacos, and casseroles.
- Add
high-calorie foods to snacks and meals. - Add higher calorie condiments to meals and snacks.
Other tips to help improve eating:
- Be as active as possible so that you will have a good appetite.
- Brush your teeth and rinse your mouth to relieve symptoms and aftertaste.
- Create a relaxing eating environment. Try adding candles and music and eating with your loved ones.
Medicine to manage appetite loss from cancer and cancer treatment
If you are not able to keep your appetite up, talk with your doctor about appetite stimulants. These are medicines that increase appetite and can cause weight gain.
Increased appetite, weight gain, and cancer
Although many people with cancer have appetite loss and lose weight, you may gain weight during cancer treatment.
Weight gain is more common if you have ovarian, breast, or prostate cancer. Each person is different, so even if you have one of these cancers, it does not mean you will gain weight. And you may gain weight if you have a different type of cancer.
If you gain weight during your cancer treatment, let your doctor know so they can assess the cause and type of weight gain. Small weight fluctuations during cancer treatment are normal and expected. But if weight gain is sudden, such as 5 pounds in a week, or does not stop, tell your doctor right away.
Causes of weight gain in people with cancer
Fluid retention. Some cancers may cause weight gain due to the size of the tumor or the buildup of fluid. There are different types of fluid buildup, but they all can cause you to gain weight. Learn more at
Increased appetite. Increased appetite and food cravings that result in weight gain may occur from the cancer itself, cancer treatment, or medicines used with cancer treatment.
Metabolic changes. Hormone therapy may cause weight gain by lowering sex hormones. When you have lower levels of sex hormones, your metabolism slows. Our metabolism is the rate at which we burn energy. A slower metabolism means you burn less energy, which makes it easier to gain weight.
Some hormone therapies and chemotherapy may lead to early menopause in women. Early menopause may decrease your metabolism and cause weight gain.
Medications. Steroids, which are often given during cancer treatment, increase appetite and make you want to eat more. When we eat more calories than our body burns, we gain weight. If you take steroids, try to eat
Steroids may also cause weight gain by causing your body to hold onto water (fluid retention). If you retain water, you may look and feel swollen. Learn more about fluid retention at
Decreased activity. Many cancer treatments can cause fatigue and pain, making it hard to be active. Being less active may in turn lead to weight gain. Talk to your doctor about how to manage problems like fatigue or pain to stay as active as possible. Learn more at
Ways to manage increased appetite and weight gain in people with cancer
Here are some tips to manage increased appetite and slow or stop weight gain. Talk with your doctor or dietitian about these tips and which ones are right for you.
Tips about foods to eat:
- Eat
foods high in fiber, such as fruits, vegetables, and whole-grain breads, cereals, and pasta. - Eat fish, lean meats, such as lean beef, pork trimmed of fat, and poultry (chicken or turkey) without skin.
- Eat plant-based proteins, such as beans, nuts, seeds, and tofu.
- Eat low-fat dairy products, such as 1% and skim.
- Eat foods that you enjoy so you feel satisfied.
Tips about foods to limit:
- Eat less fat.
- Cook with and use less salt to reduce fluid retention.
- Reduce sugary drinks like fruit juices and soda. Try diluting fruit juice with water.
- Limit or do not drink alcohol.
Grocery shopping tips:
- Buy ground meat that is 93% lean or higher.
- Buy leaner cuts of meat, such as "loin," "sirloin," or "round."
- To help control portions, buy food in single-serving containers, such as single-serve yogurts.
Meal prep tips:
- Limit cooking oils. As a general guideline, use 1 teaspoon if cooking for yourself. Use 1 to 2 tablespoons if cooking for more than just yourself.
- Use cooking methods that reduce fat, like baking, broiling, air frying, roasting, and boiling.
Other ways to help with weight gain:
- Plan meals and snacks ahead of time.
- Keep your pantry and refrigerator stocked with healthy snacks.
- Eat only when hungry.
- Find activities you enjoy, if you eat out of boredom.
- Eat more slowly. It takes about 15 minutes for the stomach and brain to know if you are full. Slowing down when you are eating can help you know if you are full or not.
- Eat smaller amounts of food at meals. Use smaller plates.
- Exercise daily.
- Keep a food diary. This can help you see what foods and drinks you eat that help you to manage your weight.
If you have swelling from steroids, try limiting or avoiding foods that are high in sodium, such as:
- breads that have a long shelf life
- sauces
- dressings
- cheese
- deli and canned meats
- olives
- certain frozen foods, such as pizza and frozen dinners
- canned foods (look for low-sodium options)
- table salt
- seasonings with salt
If you don't want to cut out these foods, look for lower sodium options. You can look at the front of a product to see if it says, "low sodium," "very low sodium," or "sodium free."
Instead of using the saltshaker, use dried or fresh spices like garlic and onion powder or fresh basil and oregano.
Talk with your doctor and dietitian before going on a diet to lose weight. If you eat because of stress, fear, or depression, think about talking with a counselor. Your doctor might also prescribe medicine to help with these feelings. Learn more about
Malnutrition and cancer
Malnutrition is when your body doesn't get enough energy, protein, vitamins, and minerals.
Causes of malnutrition in cancer
Malnutrition can be caused by the cancer itself, the side effects of cancer treatment, or both.
Cancer and its treatment can cause malnutrition in many ways. They can decrease your appetite, make you feel full quickly, and change your sense of taste and smell. These changes may cause you to eat less. In fact, decreased appetite or appetite loss is a main cause of malnutrition in people with cancer. Cancer may also lead to malnutrition by causing problems with swallowing, digestion, and absorption of your food.
Common treatment side effects that increase the risk of malnutrition are:
- appetite loss
-
dry mouth -
mouth sores - feeling full quickly
-
taste changes -
problems swallowing
Cancer and cancer treatments may also cause
Problems caused by malnutrition
Malnutrition can cause you to be weak, tired, and not able to fight infection or even finish cancer treatment. Studies show that malnutrition can decrease your quality of life and become life-threatening.
Screening for malnutrition
Your health care team may use nutrition screenings and assessments to catch eating problems early and measure your risk of malnutrition. Ask your doctor about a nutrition screening before treatment starts and when you should be screened again during treatment.
Ways to prevent malnutrition
Here are tips to prevent malnutrition.
Tips on what to eat:
- Eat
foods high in calories andprotein . - Use nutrition supplement drinks, such as Ensure or Boost.
Tips on when to eat:
- Eat small meals spaced throughout the day. Aim for five to six small meals each day.
- Eat every 2 to 3 hours.
Tips on talking with your doctor or dietitian:
- Report loss of appetite and other eating problems to your doctor right away.
- Ask your doctor about a referral to a registered dietitian. A registered dietitian can do a nutrition assessment and provide a nutrition care plan.
- Ask your dietitian about high-calorie and high-protein nutrition supplement drinks.
- Report weight loss of more than 3 to 5 pounds in one week to your doctor.
If you continue to have trouble eating and are losing weight, your doctor or dietitian might suggest tube feeding (enteral nutrition) or IV nutrition (parenteral nutrition). Learn more about tube feeding and IV nutrition at
Getting support for weight changes and malnutrition
Support from family and friends. Ask your family and friends to help with meal planning, grocery shopping, cooking, and cleaning. Provide them with a list of your favorite foods and meals they can prepare for you.
Support from your health care providers. If you're having trouble with eating and drinking, your doctor and dietitian can help. Your doctor can help you find medicines to manage certain problems and refer you to a registered dietitian. Your registered dietitian is your nutrition expert. They can help you with eating and drinking habits before, during, and after treatment.
Support for caregivers. Do not be surprised or upset if your loved one's food preferences change from day to day. There may be days when they do not want a favorite food or say it now tastes bad. Offer gentle support rather than pushing your loved one to eat. Talk with your loved one about ways to manage eating problems. Ask the doctor for a referral to a dietitian and meet with them together. Talk through problems and seek other advice that can help you both feel more in control. Learn more about getting support when your loved one is being treated for cancer at
Related resources
-
Eating Hints: Before, during, and after Cancer Treatment -
Side Effects of Cancer Treatment
What is cancer cachexia?
Cancer cachexia is a wasting syndrome that leads to weakness, fatigue, and loss of skeletal muscle (also called sarcopenia) and fat. Unlike malnutrition, it cannot be reversed with nutrition support alone. Cancer cachexia must be treated with medicines and is hard to reverse once it starts. Cancer cachexia is most common in people with advanced cancer.
There are three stages of cancer cachexia:
- Pre-cachexia. In this stage, you may have appetite loss and weight loss. Treatments for cachexia are most likely to be effective at this stage. Your doctor and dietitian will discuss how to improve your symptoms or prevent them from getting worse.
- Cachexia. You may move from pre-cachexia to cachexia depending on the type and stage of your cancer, how you respond to cancer treatment, and your eating habits. In the cachexia stage, you may lose interest in eating and continue to lose weight and muscle. Other symptoms include fatigue and reduced strength.
- Refractory cachexia. In this stage, you have severe muscle loss and continue to lose weight. Refractory cachexia affects many people with advanced cancer that is not responding to cancer treatment.
What causes cancer cachexia?
Scientists don't fully understand how cachexia occurs in people with cancer. But they think that inflammation is the main cause. Increased metabolism, insulin resistance, and hormone changes may also play roles.
Inflammation
Inflammation can cause appetite loss, loss of muscle and fat, changes in how the body uses nutrients, decreased eating, and increased metabolism. Lab tests show that certain cancers, such as breast, ovarian, and esophageal cancer, can cause inflammation in the body.
Changes in metabolism
Some cancers can change your metabolism, or how your body uses carbohydrates, protein, and fat from food. Changes may include rapid breakdown of protein and fat stores in the body, causing muscle and fat loss. An increased metabolism also means your body uses more energy. This makes it harder for your body to meet its energy and protein needs, leading to weight loss and possible cachexia.
Not all people with cancer have an increased metabolism. But it is common in those with head and neck, lung, and pancreatic cancers and cancers of the upper digestive tract.
Insulin resistance
People with cancer may have insulin resistance. Normally, after you eat food, insulin tells your cells to allow glucose (sugar) to move from your blood into your cells. But with insulin resistance, the cells no longer respond to insulin. When your cells can't respond to insulin, glucose can't enter your cells and it builds up in your blood, causing high blood sugar (a condition called hyperglycemia). And when glucose cannot get into your cells, it is not available to be used by the cells for energy. This can lead to weight loss and possible cachexia.
Changes in hormones
Cancer cachexia may also be caused by a change in hormones, chemical messengers that tell your cells what to do. Two groups of hormones are linked with cancer cachexia: catabolic and anabolic hormones. Catabolic hormones break down tissue, and anabolic hormones build tissue. In cancer cachexia, your body has more working catabolic hormones than anabolic hormones. This imbalance leads to muscle breakdown, making cancer cachexia worse.
Symptoms of cancer cachexia
The most common symptoms of cachexia are:
-
weight loss , including loss of muscle and fat -
appetite loss -
fatigue - weakness
These symptoms can have many causes and may not be a sign of cachexia. It's important to talk with your doctor if you notice these changes. Your doctor can help you manage them and decide if other tests are needed.
Ways to prevent cancer cachexia
Spotting and treating malnutrition early is the best way to prevent cancer cachexia. Talk to your doctor about regular nutrition screenings during treatment to see if you are at risk of malnutrition and cancer cachexia. Learn more at
Ways to manage cancer cachexia
You need the help of many types of health care providers to manage cachexia.
Your doctor may prescribe medicines such as appetite stimulants and anti-inflammatory drugs. They might refer you to a registered dietitian who can suggest nutrition supplement drinks, such as Ensure or Boost. Dietitians can provide nutrition counseling and education for you and your caregivers. If you need it, dietitians oversee nutrition support such as tube feeding (enteral nutrition) and IV nutrition (parenteral nutrition). Learn more about tube feeding and IV nutrition at
Your doctor might refer you to physical therapy. Physical therapy can help improve strength and endurance. Getting stronger can help you move better and take part in daily activities, which can help improve your quality of life.
If swallowing becomes an issue, your doctor can refer you to a speech therapist. If mouth sores or other mouth problems are getting in the way of eating and drinking, your doctor may suggest you see a dentist. Learn more about managing mouth problems during cancer treatment at
Getting support for cancer cachexia
Support from family and friends. Cachexia can make you feel tired and unable to do your daily activities. Reach out to your family and friends to help with meal planning, grocery shopping, cooking, and cleaning. Your family and friends will want to know how to help you. If people offer help, accept it.
Support from your health care providers. Be sure that your doctor knows about problems you are having. Your doctor can prescribe medicine and refer you to other health care providers as needed.
Support for caregivers. It is normal to feel distress when a loved one has cachexia. You might be upset about their weight loss, loss of physical function, and changing appearance.
There may be days when your loved one does not want to eat or drink. Offer gentle support rather than pushing your loved one to eat. Ask the doctor for referrals to a dietitian and physical therapist to help your loved one with cachexia. Meet with them together so you know how best to help your loved one.
Learning about cachexia can help you know what to expect, which can ease your distress. Learn more about getting support at
Cancer cachexia often happens at the end of life. To prepare, it might help to talk with the doctor or nurse about what to expect during this time. Learn more at
Related resources
-
Cancer Cachexia: After Years of No Advances, Progress Looks Possible -
Nutrition in Cancer Care (PDQ®)–Health Professional Version
Last Revised: 2024-12-11
If you want to know more about cancer and how it is treated, or if you wish to know about clinical trials for your type of cancer, you can call the NCI's Cancer Information Service at 1-800-422-6237, toll free. A trained information specialist can talk with you and answer your questions.
This information does not replace the advice of a doctor. Ignite Healthwise, LLC, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the
Healthwise, Healthwise for every health decision, and the Healthwise logo are trademarks of Ignite Healthwise, LLC.
Page Footer
I want to...
Audiences
Secure Member Sites
The Cigna Group Information
Disclaimer
Individual and family medical and dental insurance plans are insured by Cigna Health and Life Insurance Company (CHLIC), Cigna HealthCare of Arizona, Inc., Cigna HealthCare of Illinois, Inc., Cigna HealthCare of Georgia, Inc., Cigna HealthCare of North Carolina, Inc., Cigna HealthCare of South Carolina, Inc., and Cigna HealthCare of Texas, Inc. Group health insurance and health benefit plans are insured or administered by CHLIC, Connecticut General Life Insurance Company (CGLIC), or their affiliates (see
All insurance policies and group benefit plans contain exclusions and limitations. For availability, costs and complete details of coverage, contact a licensed agent or Cigna sales representative. This website is not intended for residents of New Mexico.