Treatment Option Overview
There are different types of treatment for patients with pheochromocytoma or paraganglioma.
Different types of treatments are available for patients with pheochromocytoma or paraganglioma. Some treatments are standard (the currently used treatment), and some are being tested in clinical trials. A treatment clinical trial is a research study meant to help improve current treatments or obtain information on new treatments for patients with cancer. When clinical trials show that a new treatment is better than the standard treatment, the new treatment may become the standard treatment. Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment
Patients receive medication to treat the signs and symptoms of pheochromocytoma and paraganglioma.
Drug therapy begins when pheochromocytoma or paraganglioma is diagnosed. This may include:
- Drugs that keep the blood pressure normal. For example, one type of drug called alpha-blockers stops noradrenaline from making small blood vessels more narrow. Keeping the blood vessels open and relaxed improves blood flow and lowers blood pressure.
- Drugs that keep the heart rate normal. For example, one type of drug called beta-blockers stops the effect of too much noradrenaline and slows the heart rate.
- Drugs that block the effect of extra hormones made by the adrenal gland.
Drug therapy is often given for one to three weeks before surgery.
The following types of treatment are used:
Surgery
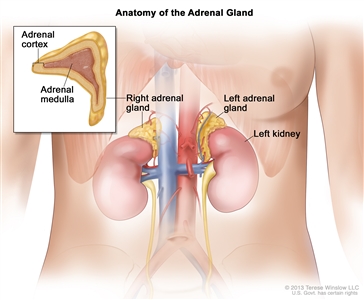
Surgery to remove pheochromocytoma is usually an adrenalectomy (removal of one or both adrenal glands). During this surgery, the tissues and lymph nodes inside the abdomen will be checked and if the tumor has spread, these tissues may also be removed. Drugs may be given before, during, and after surgery to keep blood pressure and heart rate normal.
After surgery to remove the tumor, catecholamine levels in the blood or urine are checked. Normal catecholamine levels are a sign that all the pheochromocytoma cells were removed.
If both adrenal glands are removed, life-long hormone therapy to replace hormones made by the adrenal glands is needed.
Radiation therapy
Radiation therapy uses high-energy x-rays or other types of radiation to kill cancer cells or keep them from growing.
- External radiation therapy uses a machine outside the body to send radiation toward the area of the body with cancer.
- Metastatic pheochromocytoma is sometimes treated with a radioactive substance called 131I-MIBG. It is given by infusion to deliver radiation directly to tumor cells throughout the body. 131I-MIBG collects in certain kinds of tumor cells, killing them with the radiation that is given off. Not all pheochromocytomas take up 131I-MIBG, so a test is done first to check for this before treatment begins.
The way the radiation therapy is given depends on whether the cancer is localized, regional, metastatic, or recurrent. External radiation therapy and 131I-MIBG therapy are used to treat pheochromocytoma.
Chemotherapy
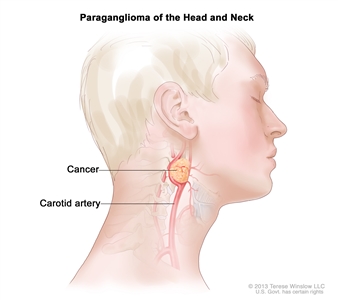
Chemotherapy is a cancer treatment that uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing. When chemotherapy is taken by mouth or injected into a vein or muscle, the drugs enter the bloodstream and can reach cancer cells throughout the body (systemic chemotherapy). Combination chemotherapy is treatment using more than one anticancer drug. Systemic chemotherapy is used to treat pheochromocytomas and paragangliomas.
Ablation therapy
Ablation is a treatment to remove or destroy a body part or tissue or its function. Ablation therapies used to help kill cancer cells include:
- Radiofrequency ablation: A procedure that uses radio waves to heat and destroy abnormal cells. The radio waves travel through electrodes (small devices that carry electricity). Radiofrequency ablation may be used to treat cancer and other conditions.
- Cryoablation: A procedure in which tissue is frozen to destroy abnormal cells. Liquid nitrogen or liquid carbon dioxide is used to freeze the tissue.
Embolization therapy
Embolization therapy is a treatment to block the artery leading to the adrenal gland. Blocking the flow of blood to the adrenal glands helps kill cancer cells growing there.
Targeted therapy
Targeted therapy is a type of treatment that uses drugs or other substances to identify and attack specific cancer cells. Tyrosine kinase inhibitors (TKIs) block signals needed for tumors to grow. Sunitinib, axitinib, and cabozantinib have been used as palliative therapy for metastatic and recurrent pheochromocytoma.
New types of treatment are being tested in clinical trials.
For some people, joining a clinical trial may be an option. There are different types of clinical trials for people with cancer. For example, a treatment trial tests new treatments or new ways of using current treatments. Supportive care and palliative care trials look at ways to improve quality of life, especially for those who have side effects from cancer and its treatment.
You can use the clinical trial search to find NCI-supported cancer clinical trials accepting participants. The search allows you to filter trials based on the type of cancer, your age, and where the trials are being done. Clinical trials supported by other organizations can be found on the ClinicalTrials.gov website.
Learn more about clinical trials, including how to find and join one, at Clinical Trials Information for Patients and Caregivers.
Treatment for pheochromocytoma and paraganglioma may cause side effects.
For information about side effects caused by treatment for cancer, visit our Side Effects page.
Follow-up care will be needed.
Some of the tests that were done to diagnose the cancer or to find out the extent of the cancer may be repeated. Some tests will be repeated to see how well the treatment is working. Decisions about whether to continue, change, or stop treatment will be based on the results of these tests.
Some of the tests will continue to be done after treatment has ended. The results of these tests can show if your condition has changed or if the cancer has recurred (come back). These tests are sometimes called follow-up tests.
For patients with pheochromocytoma or paraganglioma that causes symptoms, catecholamine levels in the blood and urine will be checked on a regular basis. Catecholamine levels that are higher than normal can be a sign that the cancer has come back.
For patients with paraganglioma that does not cause symptoms, follow-up tests, such as CT, MRI, or MIBG scan should be done every year.
For patients with inherited pheochromocytoma or paraganglioma, catecholamine levels in the blood and urine will be checked on a regular basis. Other screening tests will be done to check for other tumors that are linked to the inherited syndrome.
Talk to your doctor about which tests should be done and how often. Patients with pheochromocytoma or paraganglioma need lifelong follow-up.