CPAP and Other Devices
CPAP
Continuous positive airway pressure (CPAP) is nearly always the first medical treatment for sleep apnea. CPAP is a machine that prevents your airways from closing during sleep.
CPAP can:
- Decrease daytime sleepiness. If you still feel sleepy during the day while using CPAP at night, tell your doctor.
- Lower daytime and nighttime blood pressure.
It may take time for you to be comfortable using CPAP. You may find that you want to take off the mask, or you may find it hard to sleep. If you can't get used to CPAP, talk to your doctor. You might be able to try another type of mask or make other adjustments.
Some CPAP devices automatically adjust air pressure or use different air pressures when you breathe in or out. They are easier and more comfortable for some people to use.
Sometimes medicine that helps you stay awake during the day may be used along with CPAP.
If you use CPAP, or another machine to help you breathe, you need to use it every night and while you nap. If you don't use it, your symptoms will return right away.
Oral and nasal breathing devices
Mouth devices, nose devices, or nerve stimulation devices are sometimes used to treat obstructive sleep apnea.
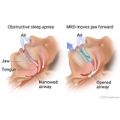
Oral devices (also called oral appliances) push the jaw or hold the tongue forward. This makes the airway larger and improves airflow. It also reduces the chance that tissue will collapse and narrow the airway when you breathe in. Oral devices may be used for people with sleep apnea who find that continuous positive airway pressure (CPAP) doesn't work for them.
Examples of oral devices include a mandibular repositioning device (MRD) or a tongue-retaining device. A dentist will shape the device to fit your mouth.
Your doctor may suggest that you use nasal devices (such as nose strips or disks) to help keep your airways open while you sleep. Nose strips widen the nostrils and improve airflow. Nasal disks have a valve that makes it harder for you to breathe out. This causes a little back-pressure in the airways that may help keep them open.
You can get many of these oral or nasal devices without a prescription. Talk to your doctor or pharmacist about your options.
A nerve stimulation device may be an option for some people. It is implanted in the upper chest with a surgery. The device senses the breathing pattern and mildly stimulates the airway muscles to keep the airway open.