Skip to main navigation
Skip to main content
Skip to footer
For
Medicare
For
Providers
For
Brokers
For
Employers
Español
For Individuals & Families:
For Individuals & Families
Medical
Dental
Other Supplemental
Explore coverage through work
How to Buy Health Insurance
Types of Dental Insurance
Open Enrollment vs. Special Enrollment
See all topics
Shop for international insurance plans
Member Guide
Find a Doctor
Log in to myCigna
Home
Knowledge Center
Wellness Library
Trabeculectomy (Filtration Surgery) for Glaucoma
Trabeculectomy (Filtration Surgery) for Glaucoma
Surgery Overview
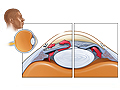
During trabeculectomy—sometimes also called filtration surgery—a piece of tissue in the drainage angle of the eye is removed, creating an opening. The opening is partially covered with a flap of tissue from the sclera, the white part of the eye, and the conjunctiva, the clear thin covering over the sclera. This new opening allows fluid (aqueous humor) to drain out of the eye, bypassing the clogged drainage channels of the trabecular meshwork.
As the fluid flows through the new drainage opening, the tissue over the opening rises to form a little blister or bubble, called a bleb. The bleb is located where the sclera, or white of the eye, joins the iris, the colored part of the eye. During office visits after surgery, the doctor looks at the bleb to make sure that fluid is still draining out of the new opening. Not all blebs have to be easily seen to work.
What To Expect
What To Expect
Most people don't have to be admitted to the hospital. But children who have the surgery may stay in the hospital overnight. And in some cases, your doctor may recommend that you stay in the hospital.
Right after surgery, antibiotics may be applied to the eye. They may also be injected under the lining of the eyelid (conjunctiva). After surgery, the eyelid is usually taped shut, and a hard covering (eye shield) is placed over the eye. A dressing is worn over the eye during the first night after surgery. You'll wear the eye shield at bedtime for up to a month. Corticosteroid medicines are usually applied to the eye for about 1 to 2 months after surgery to decrease inflammation in the eye.
You will probably have a checkup with your eye specialist the day after surgery.
Any activity that might jar the eye needs to be avoided after surgery. People usually need to avoid bending, lifting, or straining for several weeks after surgery.
After surgery, people who have problems with constipation may need to take laxatives to avoid straining while trying to pass stools. Straining can raise the pressure inside the eye (intraocular pressure). This can cause problems with the new opening that was made during surgery to drain fluid from the eye. These problems can increase the pressure in your eye even more and increase the risk of infection.
Usually there is mild discomfort after a trabeculectomy. Severe pain may be a sign of complications. If you have severe pain after your surgery, call your doctor right away.
Why It Is Done
Why It Is Done
Trabeculectomy is used to treat open-angle glaucoma and chronic closed-angle glaucoma. Trabeculectomy is usually done when medicine or laser treatment or both have failed to reduce the pressure in the eyes enough to prevent damage to a person's eyesight.
Trabeculectomy is not the first surgery used for treating children who have childhood glaucoma.
How Well It Works
How Well It Works
The new opening created by trabeculectomy allows fluid to gather under the tissue that lines the eyeball (conjunctiva), where it is absorbed into the bloodstream.
This procedure lowers pressure inside the eye. But some people need another trabeculectomy surgery or other treatments for glaucoma. Trabeculectomy is less likely to be successful in:
- Children who have congenital glaucoma.
- People who have difficult-to-control glaucoma in which new blood vessels grow on the iris (neovascular secondary glaucoma).
- People who have diabetes.
- People who have had previous eye surgery.
- People of African descent.
The long-term effectiveness of trabeculectomy surgery in preventing loss of vision from glaucoma is less certain. It is not a cure. And visual field loss can continue despite surgery.
Risks
Risks
The most common problem after a trabeculectomy is scarring of the opening. Scarring prevents fluid drainage from the eye and interferes with the proper function of the bleb. If the bleb doesn't work or causes problems, more surgery may be needed.
The medicine mitomycin is commonly used during surgery to prevent scarring. It is more commonly used than 5-fluorouracil, but it cannot be used after surgery. 5-fluorouracil can be used during the surgery or injected into the thin tissue (conjunctiva) covering the eye after surgery to prevent scarring.
Other complications of this surgery that may develop soon after surgery include:
- Bleeding in the eye.
- Sudden, permanent loss of central vision. This risk depends in part on how much central vision had been lost before surgery.
- Infection in the eye.
- High pressure in the eye, causing the space in the front part of the eye (anterior chamber) to collapse (malignant glaucoma). This is rare.
Late complications after a trabeculectomy may include:
- A cataract that is worse than it was before surgery (common).
- Continued changes in the nerve at the back of the eye related to glaucoma.
- Infection.
- Droopy eyelid (a very slight droop of the eyelid is common).
Current as of: October 1, 2025
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Ignite Healthwise, LLC education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
This information does not replace the advice of a doctor. Ignite Healthwise, LLC, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.
To learn more about Ignite Healthwise, LLC, visit webmdignite.com.
© 2024-2025 Ignite Healthwise, LLC.
<cipublic-spinner variant="large"><span>Loading…</span></cipublic-spinner>